Integrated Communication in Acute EMS Treatment: Telehealth for Pre-Hospital Acute Care
When a 911 call is placed for a medical emergency, the typical process involves dispatching EMS to the scene where initial EMS treatment takes place. Responders make their assessment, determine severity, and direct treatment based on protocols. In time-sensitive acute situations, like cases of trauma, STEMI, and stroke, the quality of that initial emergency care and the subsequent hospital care it triggers, can mean the difference between life, death, and disability. To support better patient outcomes, telemedicine and telehealth solutions are being used to provide care in the field more strategically and better direct care once patients arrive at the hospital. Here’s a closer look at the role telehealth solutions play with the three most common scenarios, and a look at the benefits it holds for all examples of acute care.
Trauma Care and Telehealth
A patient suffering severe trauma, such as internal bleeding, has a much higher chance of survival if telehealth is used both in the field through EMS treatment and at the hospital to direct their care. One study found that around 10 percent of worldwide deaths can be attributed to trauma, and with trauma centers and traumatologists primarily based in urban areas, those in rural settings are at an even greater risk of dying due to a traumatic cause. Especially in areas where specialized care is a great distance away, telehealth solutions have the potential to prevent a significant number of these deaths by helping provide timely access to resources. In part, this challenge is being addressed through a nationwide trauma transfer system, which supports the physical transfer of a patient, typically from a rural physician to a specialized trauma center. However, considering transportation barriers, the cost of such transportation, and the time spent in transfer, time-sensitive trauma injuries are best handled on-site. Telehealth solutions are helping bridge the gaps in trauma care with “teletrauma” technology. In trauma cases, telehealth helps quickly connect advanced resources and highly trained personnel to physicians working in remote settings. Telepresence gives smaller and rural facilities 24/7 access to trauma surgeons working at major trauma centers, but it extends beyond a video conference. Expert patient evaluation and guided processes help transform the level of care the patient receives, both at the time of intake and for the duration of care following. This has the potential to improve trauma patient outcomes vastly, particularly in areas where specialized trauma care is hours away.
STEMI Care and Telehealth
STEMI is a life-threatening type of heart attack that occurs when a major artery in the heart, one supplying oxygen and nutrient-rich blood to the heart muscle, becomes blocked. Typically, STEMI is associated with coronary artery disease or atherosclerosis. One of the biggest measures of quality in STEMI care is the “door-to-balloon,” which is the time it takes for the occluded artery to be successfully reopened. Traditionally, the clock starts when the patient arrives at the hospital door, but the American Heart Association is encouraging the measure to evolve to “first medical contact to balloon,” with the goal of completing the reperfusion within 90 minutes of EMS being by the patient’s side. Many more argue the clock should begin counting down from the moment the patient calls 911, and with telehealth, that may just be achievable. One way telehealth is bringing more immediate and specialized care to STEMI patients is with the use of pre-hospital 12-lead electrocardiography, patient data, and live ETA which can be transmitted by the EMS field unit to the hospital. At the hospital, telehealth and team communications again play a role, connecting cardiologists, cath teams, and STEMI coordinators. These experts can help in the diagnostics and treatment process to skip the standard emergency room triage and go straight to a cath-lab where the cardiology team is prepped and ready. Not only is this helping save lives in the United States, but it’s also playing a major role in less-developed countries. In Latin America, for instance, a one-year study implemented telehealth for rural facilities (many of which had no physician at all) and was able to reduce STEMI mortality by 55 percent. It took telemedicine professionals 11 minutes to diagnose a STEMI patient at the start of the trial, but just 3.5 minutes by the end of the trial. The average door-to-balloon time was just 48 minutes, with mortality down to 5.2 percent. This study, and many others, show that telehealth has a critical role to play in improving patient outcomes.
Stroke Care and Telehealth
Strokes occur when the brain experiences interrupted or reduced blood supply, which starves brain tissue of oxygen and nutrients. Brain cells take only minutes to die, which is why prompt treatment is critical. Even just a few minutes can make the difference between a healthy recovery and life-changing disabilities. That’s why quick administration of medications like tPA, a clot buster that can prevent brain damage, is essential. Given the dire need for fast care in stroke patients, telemedicine for strokes, called “telestroke,” has actually been used in hospitals since the 1990s. Today, video telemedicine assistance can begin in the ambulance, with a team of specialists guiding on-site responders to evaluate the patient en route to the hospital while they simultaneously prepare for the patient’s arrival. This early evaluation in EMS treatment is key because it allows the patient to skip triage and go straight to CT-scan to determine if the stroke is due to a blood clot or bleeding on the brain before treatment. Once the CT is done, neuro team stroke experts will direct care in assessing the patient, analyzing images, and determining treatment — either medication or surgery.
Embracing Telehealth for Acute Care
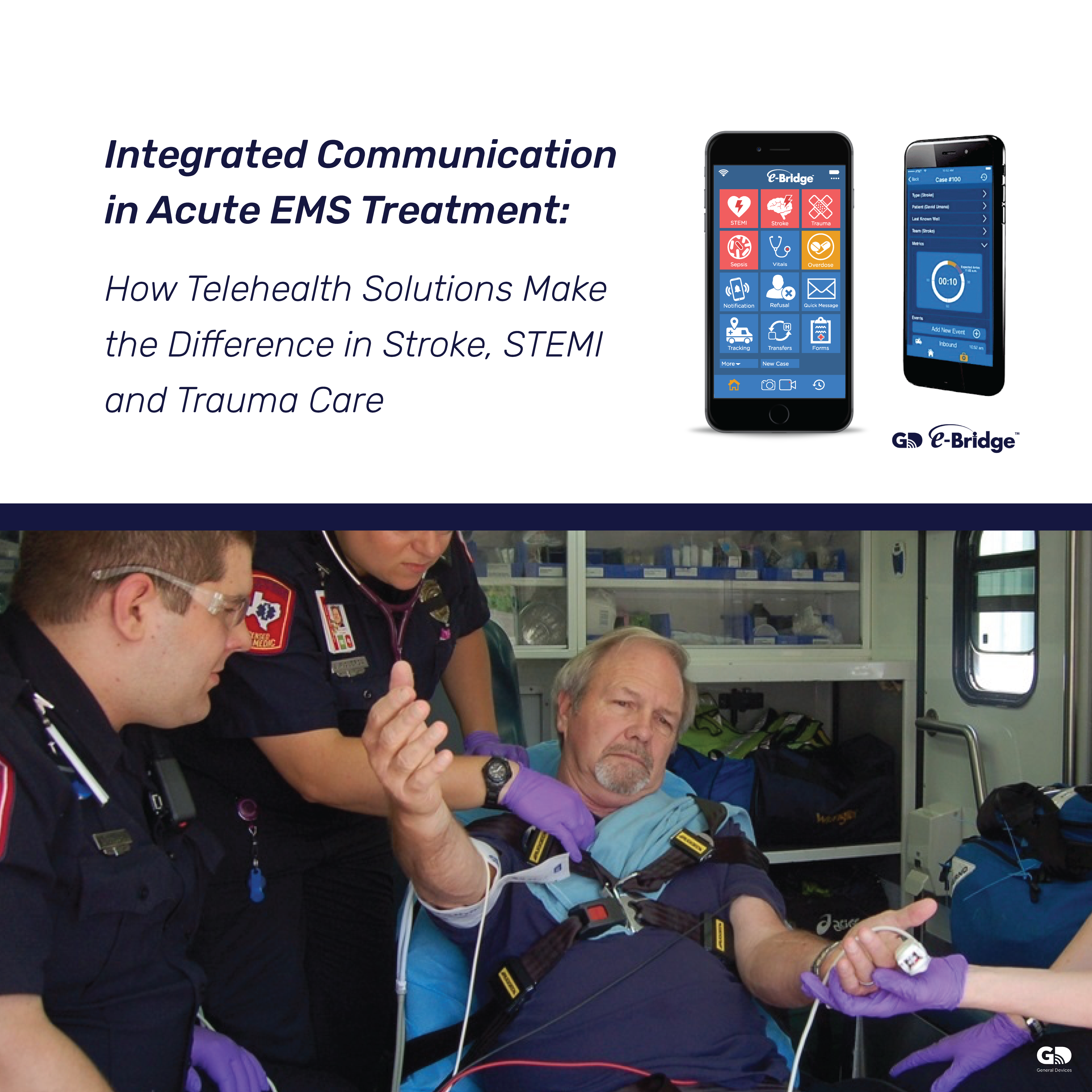
In all cases, telehealth enables even the most rural and under-funded healthcare facilities to direct patient care in an expedient and effective manner. By engaging specialized acute care teams from the moment first-responders arrive on the scene and start EMS treatment, patient outcomes can be vastly improved — particularly in cases of trauma, STEMI, and stroke, where any delay could make the difference between life and death. General Devices is leading the implementation of innovative telehealth solutions that connect EMS and hospitals to enable timely, intelligent, and cost-effective patient care. Cutting-edge solutions like e-Bridge mobile telemedicine and CAREpoint workstation are improving the treatment and outcomes for acute care, general medical, and treatment-in-place around the country.
Learn more about how they work.